A nurse is teaching a client who has a new prescription for pancrelipase to aid in digestion. The nurse should inform the client to expect which of the following gastrointestinal changes?
Decreased fat in stools
Decreased watery stools
Decreased mucus in stools
Decreased black tarry stools
The Correct Answer is A
Choice A: Decreased fat in stools
Pancrelipase is a combination of digestive enzymes, including lipase, protease, and amylase, which help break down fats, proteins, and carbohydrates. One of the primary benefits of pancrelipase is its ability to improve fat digestion and absorption. Clients with pancreatic insufficiency often experience steatorrhea, which is the presence of excess fat in stools, making them bulky, greasy, and foul-smelling. By aiding in the digestion of fats, pancrelipase reduces the fat content in stools, leading to more normal bowel movements.
Choice B: Decreased watery stools
While pancrelipase can improve overall digestion, it is not specifically known for decreasing watery stools. Watery stools can result from various conditions, including infections, inflammatory bowel disease, or other gastrointestinal disorders. Pancrelipase primarily targets the digestion of macronutrients and may not directly affect the consistency of stools unless the watery stools are due to malabsorption of fats.
Choice C: Decreased mucus in stools
Mucus in stools can be a sign of inflammation or irritation in the gastrointestinal tract, often associated with conditions like irritable bowel syndrome (IBS) or infections. Pancrelipase does not specifically target mucus production in the intestines. Its primary function is to aid in the digestion of fats, proteins, and carbohydrates, rather than addressing mucus-related issues.
Choice D: Decreased black tarry stools
Black tarry stools, also known as melena, are typically a sign of gastrointestinal bleeding, particularly from the upper GI tract. This condition requires immediate medical attention and is not related to the use of pancrelipase. Pancrelipase is not indicated for treating or preventing gastrointestinal bleeding and would not affect the presence of black tarry stools.
Free Nursing Test Bank
- Free Pharmacology Quiz 1
- Free Medical-Surgical Quiz 2
- Free Fundamentals Quiz 3
- Free Maternal-Newborn Quiz 4
- Free Anatomy and Physiology Quiz 5
- Free Obstetrics and Pediatrics Quiz 6
- Free Fluid and Electrolytes Quiz 7
- Free Community Health Quiz 8
- Free Promoting Health across the Lifespan Quiz 9
- Free Multidimensional Care Quiz 10
View Related questions
Correct Answer is A
Explanation
Choice A reason:
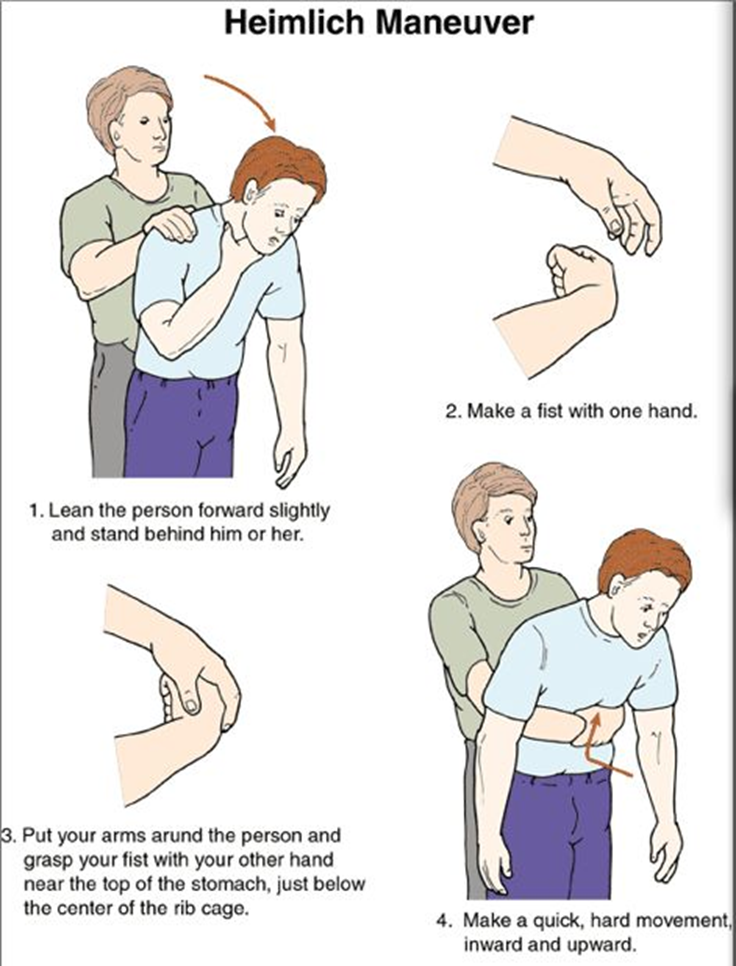
The Heimlich maneuver, also known as abdominal thrusts, is the recommended first aid technique for a conscious person who is choking. This maneuver helps to expel the object blocking the airway by using the air remaining in the lungs to force it out. The nurse should stand behind the person, place their arms around the person’s waist, make a fist with one hand, and place it just above the navel. The other hand should grasp the fist, and quick, upward thrusts should be performed until the object is expelled.
Choice B reason:
Slapping the client on the back several times is not the recommended first action for a conscious adult who is choking. While back blows can be effective, they are typically used in combination with abdominal thrusts and are more commonly recommended for infants. For adults, the Heimlich maneuver is preferred as the initial response.
Choice C reason:
Assisting the client to the floor and beginning mouth-to-mouth resuscitation is not appropriate for a conscious person who is choking. Mouth-to-mouth resuscitation, or rescue breathing, is used when a person is not breathing and is unresponsive. In this scenario, the client is conscious but unable to speak, indicating a blocked airway that requires the Heimlich maneuver.
Choice D reason:
Observing the client before taking further action is not advisable in a choking emergency. Immediate intervention is crucial to prevent the situation from worsening. If the person is unable to speak, cough, or breathe, the Heimlich maneuver should be performed without delay.
Correct Answer is A
Explanation
Choice A reason: Check the drainage for glucose:
Clear drainage from the nasal packing after a transsphenoidal hypophysectomy could indicate a cerebrospinal fluid (CSF) leak. CSF leaks are a serious complication that can occur after this type of surgery. Testing the drainage for glucose is a quick and effective way to determine if the fluid is CSF, as CSF contains glucose, whereas normal nasal secretions do not. Identifying a CSF leak promptly is crucial to prevent further complications such as meningitis.
Choice B reason: Notify the client’s provider:
While notifying the provider is important, it should be done after confirming the nature of the drainage. If the drainage is indeed CSF, the provider needs to be informed immediately. However, the initial step should be to check the drainage for glucose to confirm the suspicion.
Choice C reason: Document the amount of drainage:
Documentation is always important in nursing care, but it is not the immediate priority in this situation. The primary concern is to identify the nature of the drainage to address any potential complications promptly.
Choice D reason: Obtain a culture of the drainage:
Obtaining a culture can help identify any infections, but it is not the first step in this scenario. The immediate concern is to determine if the drainage is CSF, which requires checking for glucose.

