A nurse is caring for a client who has benign prostatic hyperplasia (BPH). The nurse should expect which of the following findings?
Painful urination
Urge incontinence
Critically elevated prostate-specific antigen (PSA) level
Difficulty starting the flow of urine
The Correct Answer is D
Choice A: Painful urination
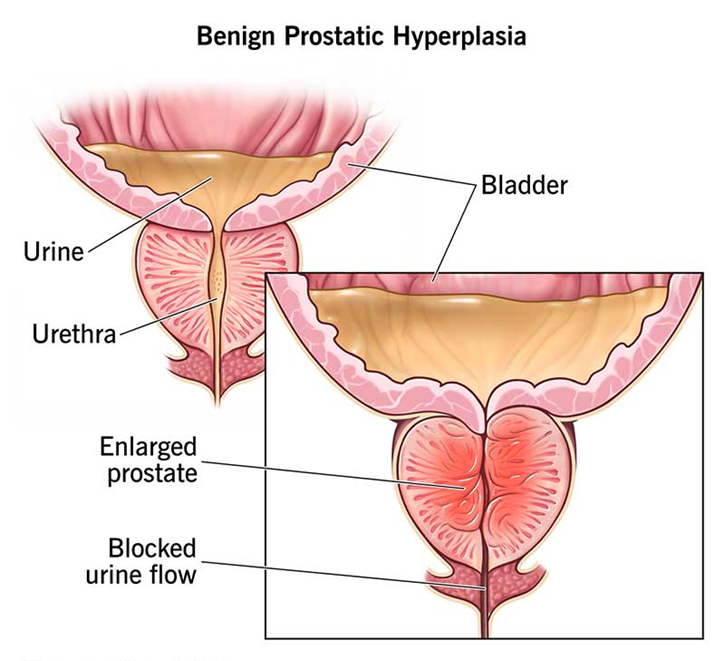
Painful urination, or dysuria, is not a typical symptom of benign prostatic hyperplasia (BPH). BPH primarily affects the flow of urine due to the enlargement of the prostate gland, which can obstruct the urethra. While BPH can cause discomfort, it does not usually result in painful urination. Painful urination is more commonly associated with urinary tract infections (UTIs) or other conditions affecting the urinary tract.
Choice B: Urge incontinence
Urge incontinence, characterized by a sudden and intense urge to urinate followed by involuntary loss of urine, can occur in some cases of BPH but is not the most common symptom. BPH typically causes symptoms related to urinary obstruction, such as difficulty starting urination, weak urine stream, and incomplete bladder emptying. Urge incontinence may develop if the bladder becomes overactive due to the obstruction, but it is not a primary symptom.
Choice C: Critically elevated prostate-specific antigen (PSA) level
While an elevated prostate-specific antigen (PSA) level can be associated with BPH, it is not a definitive finding. PSA levels can be elevated due to various conditions, including prostate cancer, prostatitis, and BPH. However, a critically elevated PSA level is more concerning for prostate cancer rather than BPH. Therefore, while PSA testing is useful in the evaluation of prostate conditions, it is not specific to BPH.
Choice D: Difficulty starting the flow of urine
Difficulty starting the flow of urine, also known as hesitancy, is a hallmark symptom of BPH. The enlarged prostate gland can compress the urethra, making it difficult for urine to pass through. This can lead to a weak urine stream, straining to urinate, and a feeling of incomplete bladder emptying. These symptoms are collectively known as lower urinary tract symptoms (LUTS) and are commonly associated with BPH.
Free Nursing Test Bank
- Free Pharmacology Quiz 1
- Free Medical-Surgical Quiz 2
- Free Fundamentals Quiz 3
- Free Maternal-Newborn Quiz 4
- Free Anatomy and Physiology Quiz 5
- Free Obstetrics and Pediatrics Quiz 6
- Free Fluid and Electrolytes Quiz 7
- Free Community Health Quiz 8
- Free Promoting Health across the Lifespan Quiz 9
- Free Multidimensional Care Quiz 10
View Related questions
Correct Answer is A
Explanation
Choice A: Explaining the procedure, risks, and benefits
Explaining the surgical procedure, including its risks and benefits, is primarily the responsibility of the surgeon. This is because the surgeon has the detailed knowledge and expertise regarding the specific procedure and can provide comprehensive information to the patient. The nurse’s role in this context is to support the patient by clarifying any information provided by the surgeon and ensuring that the patient understands the instructions. Nurses can also address any immediate concerns or questions the patient might have, but the detailed explanation of the procedure itself is outside their scope of practice.
Choice B: Reviewing preoperative instructions
Reviewing preoperative instructions is within the nurse’s responsibilities. Nurses play a crucial role in ensuring that patients understand and follow preoperative instructions, which may include fasting guidelines, medication adjustments, and other preparatory steps. This helps to minimize surgical risks and ensures that the patient is adequately prepared for the procedure. By reviewing these instructions, nurses help to reinforce the information provided by the surgical team and ensure patient compliance.
Choice C: Obtaining test results
Obtaining and reviewing test results is also within the nurse’s scope of practice. Nurses are responsible for ensuring that all necessary preoperative tests have been completed and that the results are available for the surgical team. This includes coordinating with the laboratory and other departments to obtain timely results and reviewing them to identify any potential issues that need to be addressed before surgery. This step is critical in ensuring patient safety and readiness for the procedure.
Choice D: Ensuring that a signed surgical consent form was completed
Ensuring that a signed surgical consent form is completed is a shared responsibility between the nurse and the surgeon. While the surgeon is responsible for obtaining informed consent by explaining the procedure, risks, and benefits, the nurse’s role is to verify that the consent form has been signed and documented appropriately. This verification process is crucial to ensure that the patient has given informed consent before proceeding with the surgery.
Choice E: Assessing the current health status of the client
Assessing the current health status of the client is a fundamental responsibility of the nurse. This involves conducting a thorough health assessment, including taking vital signs, reviewing the patient’s medical history, and identifying any potential risks or concerns that may affect the surgery. This assessment helps to establish a baseline for the patient’s condition and ensures that any necessary precautions are taken to promote a safe surgical outcome.
Correct Answer is D
Explanation
Choice A reason: Administer 50,000 units of heparin by IV bolus every 12 hours:
This dosage is incorrect and potentially dangerous. Heparin dosing must be carefully calculated based on the patient’s weight and coagulation test results. Standard practice involves adjusting the dose according to the aPTT levels to maintain therapeutic anticoagulation.
Choice B reason: Have vitamin K available on the nursing unit:
Vitamin K is the antidote for warfarin, not heparin. The antidote for heparin is protamine sulfate. Having the correct antidote available is crucial for managing potential bleeding complications associated with heparin therapy.
Choice C reason: Use tubing specific for heparin sodium when administering the infusion:
While it is important to use appropriate tubing for any IV medication, there is no specific tubing required exclusively for heparin sodium. Standard IV tubing is typically sufficient.
Choice D reason: Check the activated partial thromboplastin time (aPTT) every 6 hours:
This is correct. Monitoring aPTT levels is essential when administering a continuous heparin infusion. The aPTT test measures the time it takes for blood to clot and helps ensure that the heparin dose is within the therapeutic range. Regular monitoring helps prevent both under- and over-anticoagulation, reducing the risk of clotting or bleeding complications.
