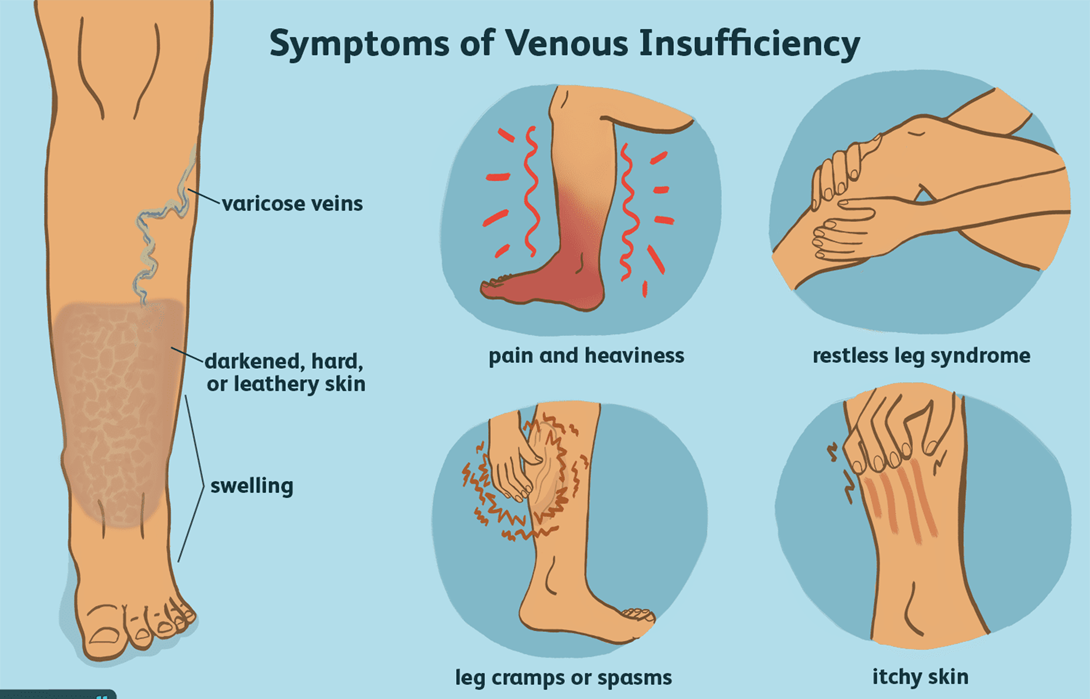
A nurse is assessing a client who has chronic venous insufficiency. Which of the following findings should the nurse expect?
Dependent rubor
Thick, deformed toenails
Hair loss
Edema
The Correct Answer is D
Choice A: Dependent rubor
Dependent rubor is a reddish discoloration of the skin that occurs when the leg is in a dependent position (hanging down). This condition is typically associated with arterial insufficiency rather than chronic venous insufficiency. Arterial insufficiency occurs when there is inadequate blood flow through the arteries, leading to symptoms such as pain, cramping, and changes in skin color. Dependent rubor is a sign of poor arterial circulation and is not commonly seen in venous insufficiency.
Choice B: Thick, deformed toenails
Thick, deformed toenails can be a sign of fungal infections or other conditions affecting the nails, but they are not specifically indicative of chronic venous insufficiency. While individuals with chronic venous insufficiency may have poor circulation that can contribute to nail problems, this symptom is not a primary or common finding associated with the condition. Instead, it is more often related to other underlying health issues.
Choice C: Hair loss
Hair loss on the legs can occur due to various reasons, including poor circulation. However, it is more commonly associated with arterial insufficiency rather than chronic venous insufficiency. In arterial insufficiency, the reduced blood flow can lead to hair loss, shiny skin, and other changes in the lower extremities. Chronic venous insufficiency primarily affects the veins and leads to symptoms such as swelling, varicose veins, and skin changes.
Choice D: Edema
Edema, or swelling, is a hallmark symptom of chronic venous insufficiency. This condition occurs when the veins in the legs are unable to effectively return blood to the heart, leading to blood pooling in the lower extremities. The increased pressure in the veins causes fluid to leak into the surrounding tissues, resulting in swelling. Edema is often more pronounced at the end of the day or after prolonged periods of standing or sitting. Managing edema is a key aspect of treating chronic venous insufficiency, and it often involves the use of compression stockings, elevation of the legs, and other measures to improve venous return.
Free Nursing Test Bank
- Free Pharmacology Quiz 1
- Free Medical-Surgical Quiz 2
- Free Fundamentals Quiz 3
- Free Maternal-Newborn Quiz 4
- Free Anatomy and Physiology Quiz 5
- Free Obstetrics and Pediatrics Quiz 6
- Free Fluid and Electrolytes Quiz 7
- Free Community Health Quiz 8
- Free Promoting Health across the Lifespan Quiz 9
- Free Multidimensional Care Quiz 10
View Related questions
Correct Answer is B
Explanation
Choice A reason: Draw sheet:
A draw sheet can be used to assist in repositioning a patient, but it is not the most effective method for turning a client who has undergone spinal fusion. The primary concern is to maintain spinal alignment, which is best achieved through the log roll technique.
Choice B reason: Log roll:
The log roll technique is the preferred method for turning patients who have had spinal surgery. This technique involves moving the patient as a single unit, keeping the spine in alignment to prevent any twisting or bending that could disrupt the surgical site. It is especially important for obese patients to ensure that the spine remains stable during movement.
Choice C reason: Sliding board:
A sliding board is typically used to assist with transfers from one surface to another, such as from a bed to a wheelchair. It is not suitable for turning a patient in bed, particularly one who has had spinal surgery.
Choice D reason: Hoyer lift:
A Hoyer lift is a mechanical device used to lift and transfer patients who are unable to move themselves. While it can be useful for transferring patients, it is not designed for turning patients in bed and does not provide the necessary support to maintain spinal alignment during a turn.
Correct Answer is ["B","D","E"]
Explanation
Choice A: Wash raw carrots before cooking
Reason: Washing raw vegetables, including carrots, before cooking is essential to remove dirt, bacteria, and pesticide residues. However, this option is not specific to preventing foodborne illnesses. Washing vegetables is a general hygiene practice, but it does not address the broader aspects of food safety, such as preventing cross-contamination or ensuring proper cooking temperatures. Therefore, while important, it is not the most critical instruction for preventing foodborne illnesses in this context.
Choice B: Separate raw foods from ready-to-eat foods
Reason: Separating raw foods from ready-to-eat foods is crucial to prevent cross-contamination. Raw foods, especially meats, poultry, and seafood, can harbor harmful bacteria that can transfer to ready-to-eat foods if not kept separate. This separation should be maintained during storage, preparation, and cooking. For example, raw meat should be stored on the bottom shelf of the refrigerator to prevent juices from dripping onto other foods. Using separate cutting boards and utensils for raw and ready-to-eat foods further minimizes the risk of cross-contamination.
Choice C: Wash utensils with warm water
Reason: While washing utensils with warm water is a good practice, it is not sufficient on its own to ensure food safety. Utensils that have come into contact with raw meat, poultry, or seafood should be washed with hot, soapy water and sanitized to kill any harmful bacteria. Simply using warm water may not effectively remove or kill bacteria, making this option less critical compared to others that directly address foodborne illness prevention.
Choice D: Practice good hand washing after handling raw eggs, meat, or poultry
Reason: Practicing good hand washing after handling raw eggs, meat, or poultry is one of the most effective ways to prevent foodborne illnesses. Hands can easily transfer bacteria from raw foods to other surfaces, utensils, and foods. Proper hand washing involves scrubbing hands with soap and water for at least 20 seconds, ensuring all parts of the hands are cleaned. This practice helps to eliminate harmful bacteria and reduce the risk of cross-contamination.
Choice E: Ensure all food is cooked to 165°F. Promptly refrigerate foods when finished eating
Reason:Cooking food to the proper internal temperature is essential to kill harmful bacteria that can cause foodborne illnesses. For most foods, an internal temperature of 165°F (73.9°C) is recommended to ensure safety. Using a food thermometer to check the temperature is the best way to ensure food is cooked thoroughly. Additionally, promptly refrigerating foods after eating helps to prevent bacterial growth. Bacteria can multiply rapidly at room temperature, so refrigerating leftovers within two hours (or one hour if the temperature is above 90°F) is crucial for food safety.